TMJ Disorders
What Is TMJ?
The TMJ, Temporomandibular Joint or jaw joint is often associated with several painful areas of the jaw, neck, sinuses, teeth, etc… Whenever there is pain in one of these areas, it is sometimes called TMD or Temporomandibular Disorder. These joints located on each side of the head in front of the ears are probably the most used and sophisticated joints of the body while talking, chewing, singing, and swallowing. It is more correct to incorporate all of these symptoms under the dental category of craniofacial pain or orofacial pain instead of "TMJ" or "TMD". However, that being said, there are specific disorders related to the TMJ primarily capsulitis, synovitis, arthritic conditions, and disc displacements.
Muscles attachments of the jaw, head, and neck will often become stiff or painful with a TMJ Disorder. Each TMJ has a small disc which allows smooth movement of the jaw when functioning and protection during compression. Disc disorders can be a cause of bite changes, annoying noises, or locking jaws. When the chewing muscles and jaw joints do not function properly together, it sometimes leads to moderate or severe pain and headaches.
Many headaches and even migraines can be a result of a temporomandibular disorder. If you suffer with headaches, dizziness, jaw fatigue, earaches, facial pain, difficulty in closing the teeth together, pain when chewing or neck and shoulder stiffness, it may be TMJ disorder. It is estimated as many as one in every four Americans suffers from one or more symptoms of a TMD. While the majority of sufferers are women; men and adolescents also suffer with symptoms.
Common symptoms are: headaches, migraine, jaw pain, jaw joint noises, neck pain, neck stiffness, ear pain, and ear stuffiness, and decreased jaw or neck range of motion.
Do I Have Disc Displacement?

MRI of a normal TMJ
A properly positioned disc does not usually create any noise (popping, clicking, or grinding).

Mandibular disk displacement
Many people are aware of having jaw joint noises. They are caused from the disc being out of position (a disc displacement). Disc displacements are common in the population, and most don't require a treatment. Usually, the disc displacement is not the source of pain even though it might be painful to pop.
Popping can occur very softly and unnoticed or very loudly. The degree of noise can depend on the amount of muscle tension in the face as well as the shape of the disc and joint fossa.
What Causes a Disc Displacement?
A disc displacement is almost always caused by trauma even from childhood and can go unnoticed until a later time when the face muscles become tense from numerous reasons.
There are many causes like trauma (blow to the head, whiplash), malocclusion (bad bite or missing teeth), poor posture, bruxism (teeth grinding) or skeletal malformation, arthritis in the joint or clenching brought on by stress. Anything that keeps these muscles, bones and joints from working together harmoniously is called TMJ disorder.
Do I have TMJ arthritis?
The diagnosis can be made from radiographs preferably a CT or MRI.
Symptoms associated with TMJ arthritis may include headaches, jaw pain, limited opening, jaw locking, ear pain, ear congestion, neck pain or tension, pain behind the eyes, joint noise and more. It is imperative that you be screened by a dentist trained and experienced in these disorders. Treatment is usually indicated when you suffer with any of these symptoms listed:

Decreased posterior joint space can lead to a synovitis which may cause:
- Headaches
- Teeth that do not meet properly
- Dizziness
- Difficulty chewing or swallowing
- Ringing or stuffiness in the ears
- Pain or pressure behind eyes
- Shoulder stiffness
- Facial Pain
- Limited opening of the jaw
- Jaw clicking or pain
- Jaw goes to one side when opening
- Neck pain
- Tingling or numbness in arms
- Teeth sensitive to cold
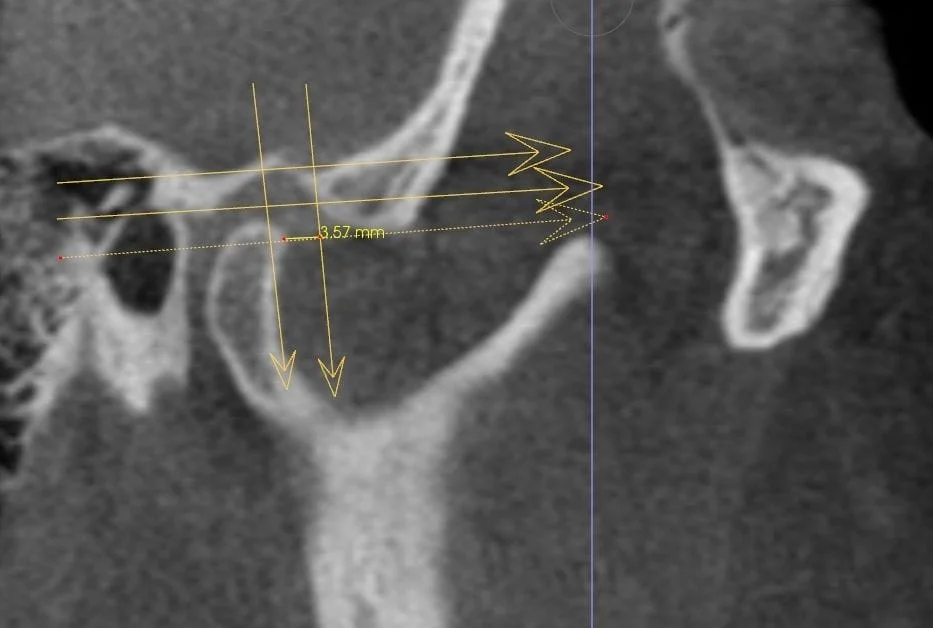
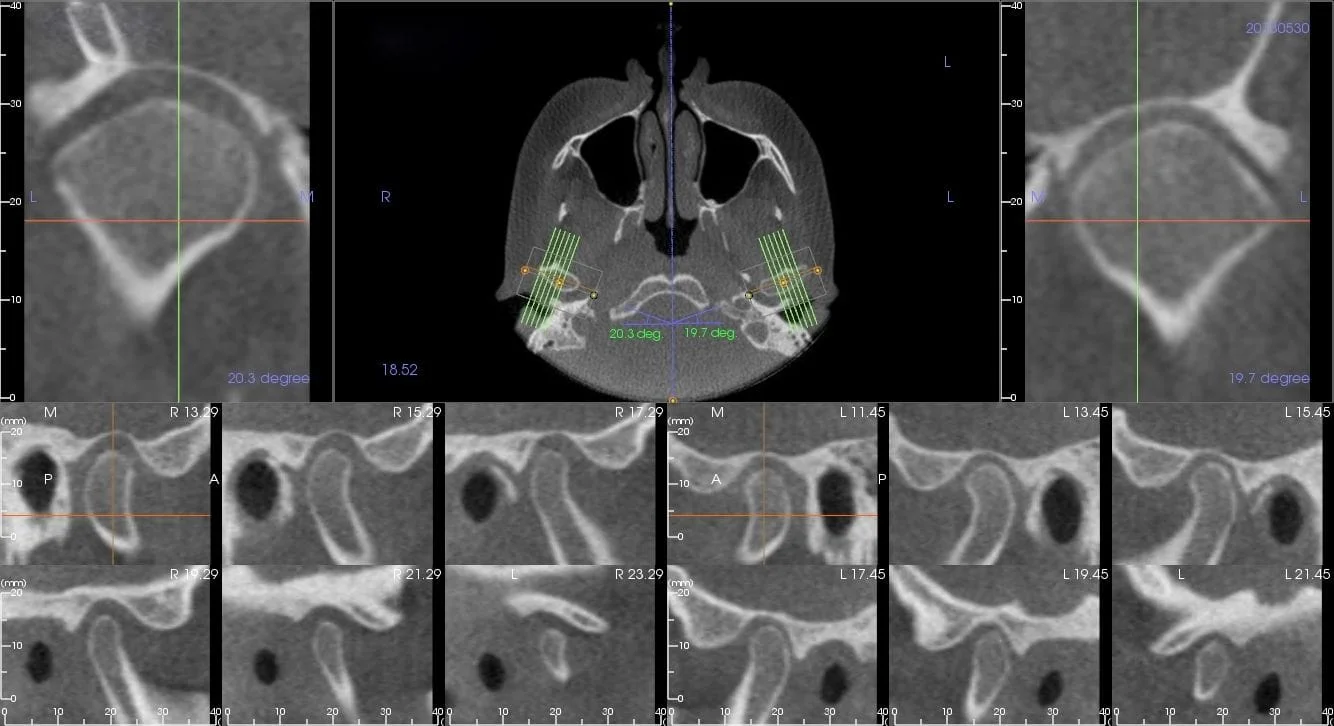
Condyle,Fossa descrepancies
Diagnosing TMJ Disorders
Severe TMJ arthritis
Temporomandibular Joint Disorders (TMD/TMJ) can be difficult to diagnose, because the problem may be generated by several sources and can create a situation where different providers need to work together. Arthritis is for sure one of the most difficult to treat. TMJ arthritis treatment may involve appliances, medication, arthrocentesis, arthroscopy, or even joint replacement.
People who suffer with TMD disorders have typically visited many different health care professionals -- all of whom may have a piece of the puzzle, yet they continue to have problems with their TM joints. To properly diagnosis a TMD disorder several possibilities need to be considered and that requires an examination that is more than looking at the teeth.
ADVANCED STATE-OF-THE-ART EQUIPMENT:
Dr. McCarty has been trained in the use of JVA, Jaw Tracking, EMG and received a Mastership certificate from BioPAK in 2004, however, he currently has replaced these techniques with others. A wide range of diagnostic methods are available to identify head, neck, facial and TMJ problems. Each method is used only as needed in each individual case. These tests might include:
- JVA – Joint Vibration Analysis
- Jaw tracking computerized equipment
Dr. McCarty has been trained in the use of JVA and Jaw Tracking which is a useful tool to estimate an existing disc displacement and the location of the reduction in the patient's opening. Other tools that can be useful for listening for joint sounds include doppler, stethoscope, and microphone devices. JVA/JT is only a tool, but along with doppler appears to be the best available. MRI and surgically opening the joint are the only ways to visualize a disc.
- EMG – Electromyography
Dr. McCarty was trained in the use of surface EMG for determining muscle hyperactivity, and the use with TENS in taking neuromuscular bites years ago and in fact received a mastership from BioPak certifying his ability to understand and use that technology; however he stopped using that technology approximately 14 years ago as he found other means of treating that he feels are more effective.
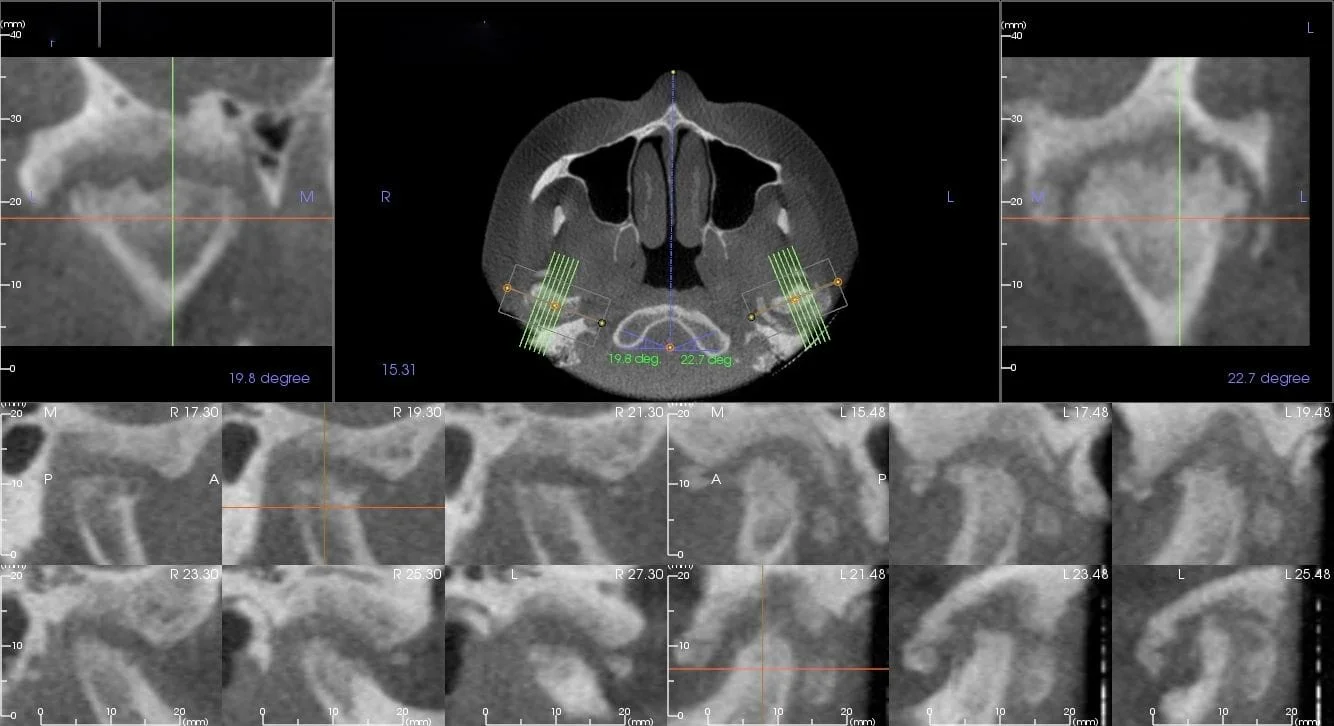
- Cone Beam CT scanning (CBCT)
Dr. McCarty believes the CBCT is essential for a proper diagnosis. There are cases where sinus infections or tooth infections are mimicking TMJ symptoms. There are cases where upper cervical pain or even cancer are mimicking TMJ symptoms. Dr. McCarty has seen all of these situations and without this proper knowledge gained by the CBCT, the wrong assessment can easily be made leading to the wrong treatment plan. Many dentists will use splint therapy when there are TMJ symptoms, especially when accompanied by joint noises, and yet the problem may be generated by a completely different cause.
Treating TMJ Disorders
Dr. McCarty will typically use appliance therapy to unload a painful TMJ. This will be used in combination with anti-inflammatories. Anti-inflammatories may be given orally, by injection, by Iontophoresis, or PRF (Platelet-Rich Fibrin). If the TMJ does not respond to these treatments a referral to the oral surgeon for possible arthrocentesis or arthroscopic procedures.
Below is a list of procedures commonly used:
- Appliances (Used for different reasons)
- Trigger Point Injections (Used to break up Trigger Points)
- Steroid Injections
- Platelet-Rich Fibrin (PRF)
- High Voltage Stimulation (Occasional use for Trigger Points or to break muscle spasm.)
- Ultrasound (Occasional use for myositis or temporal tendonitis.)
- Iontophoresis (Occasionally used for TMJ lateral pole inflammation.)
- Spray & Stretch (Used to break up Trigger Points or for diagnosis.)
- Prolotherapy (Used to reduced pain at ligaments or tendon insertions.)
- TENS (Rarely used except for temporary pain relief.)
- Medications (Temporarily use to reduce muscle spasm, inflammation, & decrease parafunction.)
- Cold Laser (Occasionally used to reduce pain and inflammation.)
- Surgical referral options (For arthroscopic procedures, disc plication, arthrocentesis, and occasional joint replacement.)
Orthotics:
A custom fitted orthotic is often a suggested form of treatment. Dr. McCarty believes the orthotic is primarily used to unload a painful inflamed source much like crutches or an ankle boot would unload a sprained ankle. Appliances in the mouth can also influence upper cervical posture helping to reduce occipital nerve pain. Appliances during sleep can change a person's parafunction habits and improve airways. Appliances can also be used to reduce or recapture a disc in some cases, and that process usually requires a phase 2 stabilization. Dr. McCarty refers to other providers for phase 2 stabilization in his practice but did complete phase 2 years ago and understands the process. Since phase 2 is not performed in his practice, he has no incentive for recommending phase 2 unless really deemed necessary. He finds that the phase 2 process is rarely needed, and most of his patients are able to maintain stability and remain comfortable with long term night appliances after they are treated.
Photo below depicts a normal TMJ morphology.