Orofacial Pain
What Is Orofacial or Craniofacial Pain?
The specialty of Orofacial Pain Dentistry is concerned with the prevention, evaluation, diagnosis, treatment, and rehabilitation of orofacial pain disorders or sometimes called TMD disorders. The word Craniofacial Pain has been used interchangeably with Orofacial Pain for many years. The terms orofacial and craniofacial should not confuse the patient seeking help.
Orofacial Pain encompasses such issues that cause head and neck pain that is often non-tooth related. It mimics TMJ problems and may also cause indirect jaw and joint dysfunction due to the pain and muscle spasm associated with it. It involves treatment of neurovascular and tension type headaches and jaw symptoms. It involves muscle, tendon, and ligament injuries in the face.
Orofacial pain is evolving and the scope of the field is enlarging. At the present time, orofacial pain encompasses:
- Masticatory musculoskeletal pain
- Cervical musculoskeletal pain
- Neurovascular pain
- Neuropathic pain
- Sleep disorders related to orofacial pain
- Intraoral
- Intracranial
- Extracranial
- Orofacial Dystonias
- Headaches
- Migraines
- Facial Pain
Symptoms of Orofacial Pain
Oral facial pain includes a number of clinical problems which may include but are not limited to the following:
- Temporomandibular Disorders
- Myofascial Pain (Muscle Trigger Points)
- Muscle Spasm
- Headaches
- Migraine
- Oral Pain from teeth, gums, or bones
- Craniofacial Pain Syndromes like:
- Temporal Tendonitis
- Ernest Syndrome
- Hamular Bursitis
- Occipital Neuritis
- Arthritis (TMJ and Cervical)
- Trigeminal Neuralgia
- Cervicalgia
- Anxiety
- Depression
- Fibromyalgia
- Muscle movement Disorders (Dystonias)
Diagnosis of Orofacial Pain
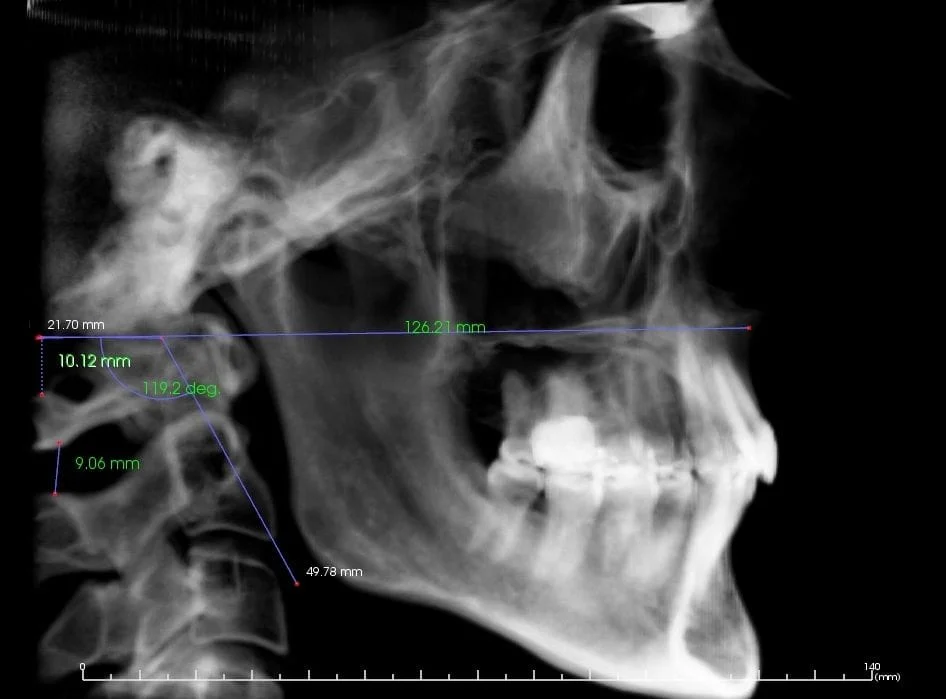
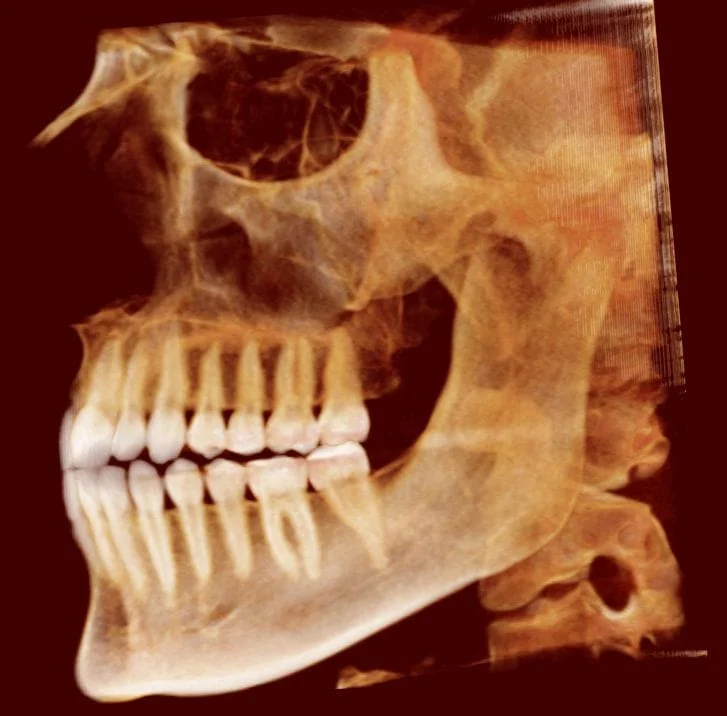
Abnormal cervical relationship (Can be a clue to cervical generated pain)
A careful consideration needs to be made in the diagnosis of TMD and orofacial pain which often is time consuming. This is extremely difficult in the everyday dental office which has concerns for clean teeth, cosmetic procedures, fillings, root canals, dentures, tooth whitening, and everything else.
This is the primary reason it can be important to seek out a dentist who spends all of his or her time dealing with only TMD and orofacial pain. By taking into consideration the history and findings of the complete examination and often by using diagnostic blocks of nerves, a proper diagnosis can be made. A proper treatment plan cannot be established without a proper diagnosis, which is what almost 100% of the patients presenting to a TMJ office don’t have when they arrive.
The special needs of the pediatric and geriatric populations are considered when formulating a comprehensive treatment plan for these patients. Dr. McCarty will make a diagnosis on the basis of a detailed assessment of the character of the pain, including: duration, site, severity, character, frequency and periodicity, associated features, initiating factors and relieving factors.
We will take a medical and dental history to determine if any trauma has occurred in the facial area, perform a physical examination to examine your temporomandibular joint and look at head and neck structure. Maintaining or correcting your bite ensures optimal health and proper care, which will help reduce or eliminate orofacial pain or discomfort.
Treatment of Orofacial pain
Dr. McCarty's objective is to locate the source of the pain and alleviate it. What is confusing about face pain is there are several sensory inputs to the trigeminal nerve system that "cross-talk" and produce similar muscle responses. The pain may be originating from any of the trigeminal branches including any superficial or deep facial structures (teeth, gums, TMJs, bones, sinuses, skin, etc....), upper cervical areas including the C1-C3 nerves and possibly lower cervical nerves (shoulders and up), and throat. Since all 3 branches of the Trigeminal N., C1-C3, the Glossopharyngeal N., the Facial N, and the Vagus N. all contribute sensory input to the Trigeminal Nucleus, not only is there cross-talk, but also similar motor responses in the 3rd division of the Trigeminal N. Therefore, we may see muscle tension and pain in muscles like the: masseter, temporalis, lateral pterygoid, medial pterygoid, mylohyoid, anterior digastric, tensor tympani, and tensor veli palatini. Tension of these muscles will lead to bite changes, stuffy ears (as the tensor veli palatini and levator veli palatini are involved in ear congestion), and trigger point formation. In my opinion many of the cases we see are from upper cervical pain and from trapezius or Sternocleidomastoid trigger points. Many dental providers fail to find the source of the pain and treat facial pain as a bite problem. This can lead to very expensive treatment plans. There are different ways to alleviate pain sources which may include the following:
Treatments include:
- Appliances (Used for different reasons.)
- Physical Therapy Modalities
- High Voltage Stimulation (Occasional use for Trigger Points or to break muscle spasm.)
- Ultrasound (Occasional use for myositis or temporal tendonitis.)
- Iontophoresis (Occasionally used for TMJ lateral pole inflammation.)
- Spray & Stretch (Used to break up Trigger Points or for diagnosis.)
- Cold Laser (Occasionally used to reduce pain and inflammation.)
- TENS (Rarely used except for temporary pain relief.)
- Injections
- Trigger Point Injections (Used to break up Trigger Points.)
- Prolotherapy (Used to promote ligaments or tendon insertion repair.)
- Steroid Injections (Used to decrease inflammation)
- PRF (Platelet-Rich Fibrin) (Regenerative and anti-inflammatory)
- Botox (Used to decrease uncontrolled spasm).
- Medications (Temporarily use to reduce muscle spasm, inflammation, & decrease parafunction.)
- Surgical referral options (For arthroscopic procedures, disc plication, arthrocentesis, and occasional joint replacement.)
Botox? Dr. McCarty has had Botox training but does not recommend its use except in rare circumstances. Botox addresses the wrong end of the problem in most cases, is expensive, and it has to be repeated. I have found most individuals offering Botox as an initial treatment are not very equipped at treating orofacial pain.
Botox Review:
- Managing Temporomandibular Disorders:
- 14 Randomized controlled studies were analyzed with the findings: “The current body of research on utilizing botulinum toxin (BTX) to manage temporomandibular disorders (TMDs) has not yet yielded definitive conclusions…. Results of the meta-analysis for pain reduction were statistically insignificant for the BTX group…. BTX treatment was not significantly better than placebo for a reduction in pain scores at 1, 3, and 6 months…. There was also no difference in the effectiveness of BTX compared to placebo and other treatments for maximum mouth opening, bruxism events, and maximum occlusal force.”[1]
- Managing Orofacial Neuropathic Pain:
- All the studies demonstrated that BTX had a statistically significant efficacy in pain management compared to placebo and lidocaine.[2]
- Managing Myofascial Pain (Trigger Points): The efficacy of botulinum toxin for management of myofascial pain disorder (MPD) is controversial.[2]
- A recent study (2024) looked at 75 individuals (86% female) having myofascial pain in the masseter and temporalis. About half were treated with OnabotulinumtoxinA and half with placebo (saline). There were no statistical differences, both equally reduced pain and improved jaw function.[3]
- A 2024 study with 22 patients having MPD were equally divided. Half received Botox A delivered by iontophoresis and half with saline delivered by iontophoresis. There were no significant differences in the outcome.[4]
- A 2021 study comparing masseter injections for myofascial pain of local anesthetic, Botox, and PRP. At 3 months the local anesthetic and Botox groups were significantly better. At 6 months there seemed to be more improvement for the Botox group using a Jaw Functional Limitation Scale and a quality of life scale called OHIP-14.[4]
- Managing Bruxism and masseter hypertrophy:
- A study compared various formulations of botulinum toxin type A including onabotulinumtoxin A, abobotulinumtoxin A, and incobotulinumtoxin A. PraBTX-A (Prabotulinumtoxin A) a new type of botulinum toxin A derived from wild-type Clostridium botulinum was believed to be safe and effective treatment for bruxism and masseter hypertrophy.[5]
- Contraindications:
- “It is widely believed that the effect of BoNT on nerves and muscles of the face and jaw is temporary (Naumann, Albanese, Heinen, Molenaers, & Relja, 2016). Indeed, the prescribing information of the most-used product advises re-injection every 3–4 months for most applications (Allergan, 2020) …Histological observations of rabbit and human masseters 3–4 months postinjection suggest that not only do fiber dimensions and type remain abnormal, but fibers may degenerate (Kim, Chung, Park, & Park, 2005; Korfage et al., 2012). After a single injection, ultrastructural damage in human masseters is still severe at 6 months, although improved at 12 months (Ma, Zhai, Zhu, & Tang, 2018). With the cumulative effect of multiple injections (Kim et al., 2010), changes may become permanent…. Furthermore, paralysis of one muscle changes motor patterns such as chewing, causing modifications in other muscles (Korfage et al., 2012; Tsai, Lin, Su, Yang, & Chiu, 2012) … It is unknown if the changes in neuromuscular function and masseter histology are ultimately reversible, nor whether the human masseter reacts similarly. Nevertheless, these potential negative effects of BoNT application serve as a caution that this treatment may lead to permanent damage to neuromuscular function, or at the very least, a longer recovery than currently suggested.”[6]
- Masseter only Botox injections stiffened the temporalis muscle, and the study concludes you should perhaps do both; however, it does not consider the same effect on the medial pterygoid muscle. It implies that which ever elevator muscle not injected will be overactivated.[7]
- Side effects include pain at the injection site, localized swelling, bruising, headache, chewing weakness and aching, and the development of an asymmetric smile.[8 9]
- 1. Saini RS, Ali Abdullah Almoyad M, Binduhayyim RIH, et al. The effectiveness of botulinum toxin for temporomandibular disorders: A systematic review and meta-analysis. Plos one 2024;19(3):e0300157
- 2. Val M, Delcanho R, Ferrari M, Guarda Nardini L, Manfredini D. Is Botulinum Toxin Effective in Treating Orofacial Neuropathic Pain Disorders? A Systematic Review. Toxins 2023;15(9):541
- 3. Reeve GS, Insel O, Thomas C, Houle AN, Miloro M. Does the Use of Botulinum Toxin in Treatment of Myofascial Pain Disorder of the Masseters and Temporalis Muscles Reduce Pain, Improve Function, or Enhance Quality of Life? Journal of Oral and Maxillofacial Surgery 2024;82(4):393-401
- 4. Yilmaz O, Sivrikaya EC, Taskesen F, Pirpir C, Ciftci S. Comparison of the efficacy of botulinum toxin, local anesthesia, and platelet-rich plasma injections in patients with myofascial trigger points in the masseter muscle. Journal of Oral and Maxillofacial Surgery 2021;79(1):88. e1-88. e9
- 5. Jung BK, Park H, Cheon YW, et al. Clinical investigation of botulinum toxin (prabotulinumtoxin A) for bruxism related to masseter muscle hypertrophy: A prospective study. Journal of Cranio-Maxillofacial Surgery 2023;51(5):332-37
- 6. Baldwin MC, Liu ZJ, Rafferty KL, et al. Botulinum toxin in the masseter muscle: Lingering effects of denervation. The Anatomical Record 2022;305(5):1215-30 doi: https://doi.org/10.1002/ar.24756[published Online First: Epub Date]|.
- 7. Mierzwa D, Olchowy C, Olchowy A, et al. Botox therapy for hypertrophy of the masseter muscle causes a compensatory increase of stiffness of other muscles of masticatory apparatus. Life 2022;12(6):840
- 8. Ng ZY, Yang T. A Simple Botulinum Toxin Injection Technique for Masseter Reduction. Aesthetic surgery journal 2021;41(12):NP2104-NP05
- 9. Yeh YT, Peng JH, Peng HP. Literature review of the adverse events associated with botulinum toxin injection for the masseter muscle hypertrophy. J Cosmet Dermatol 2018;17(5):675-87 doi: 10.1111/jocd.12721[published Online First: Epub Date]|.

Teeth in proper alignment (A normal bite does not equal pain free).
